Dr. Renato Calabria, pioneer of the Stem-Cell Enhanced Facelift has unveiled before and after pictures of the procedure he performed in Florence, Italy earlier this Spring. While it’s still early, the results will only get better over time!
Here Dr Calabria explains the procedure:
For decades plastic surgeons have been looking to restore a more youthful look on the face. Surgical techniques have been improving, newer lasers have been used in order to achieve a goal that seemed unreachable. Comparing the post-operative results with the pictures of the patients when they were younger, it appeared that there was something missing: a younger face had more volume and the skin just looked fresher.
Dr. Calabria always thought that with the advent of stem cell research, plastic surgery could beneficiate from it. Using stem cell as a mean to jump start the regenerative process in our own body was definitely a very attractive proposition.
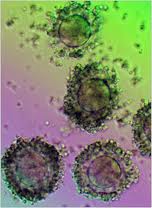
We knew that the fat in our body contained adult stem cell along with other regenerative cells. Dr. Calabria has been using fat grafting ( therefore containing adult stem cells) on the face with the distinct purpose to rejuvenate the skin and adding volume.
But was not till the develop of a new device, the Celution Device, that facial rejuvenation could taken to the next level and finally create a really amazing result.
Dr.Calabria has called this new way of the future the “cell-enhanced face lift”.
The (stem) cell-enhanced face lift is a new procedure used to volumizing the face and create a more youthful look.
Beverly Hills Plastic Surgeon Dr. Renato Calabria believes that traditional face lift should be a thing of the past: they caused the so called “wind tunnel “look by pulling tight the skin in the wrong direction. Adding volume to the face has always been Dr. Calabria’s goal. First with the Vertical Face lift, by moving the patient’s own tissues in a vertical direction and therefore repositioning it to the original and more natural position, Dr Calabria has been creating a more youthful look. And now with the (stem) cell-enhanced face lift, Dr. Calabria think he has definitely found the answer.
The (stem) Cell-Enhanced face lift not only restores the volume in the face but also adds regenerative cells which are believed to be beneficial to the rejuvenation process.
Dr. Calabria has developed a technique by which the cells are injected into the SMAS and underneath the facial musculature to create a more youthful volume adding result.
The (stem) cell-enhanced face lift combines soft tissue that is transferred from one part of the body to the face with the patient’s own adipose tissue-derived stem cells and regenerative cells.
The technique first consists of harvesting the cells ( Usually from the lower abdomen). Liposuctioned fat is rich with regenerative cells which include adult stem cells, blood vessel producing cells, growth factor secreting cells. Once the fat is harvested, it is treated through a device to isolate the cells.
Celution® Technology – How it Works
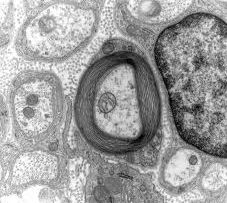
First, adipose tissue is taken from the patient by a low volume tissue collection procedure. Next, the collected tissue is placed in the Celution® Device, which processes each patient’s tissue with a single-use, application-specific consumable set that easily attaches to the Celution® Device.
The Celution® Device liberates the stem and regenerative cells from the adipose matrix; the cells are then separated, washed, and concentrated in the collection container. This real-time processing takes place in a closed environment to minimize the risk of exposure to contaminants and can be completed within the timeframe of a single surgical procedure.
Next, a syringe is used to collect the cells that are to be redelivered to the same patient. The cells may be injected directly into a site or implanted with a delivery matrix or scaffold to improve performance, such as combining the cells with an adipose tissue graft in reconstructive surgery procedures.
Following re-infusion into the body, it is thought that environmental cues from the damaged and surrounding tissue guide the stem and regenerative cells to the area of damage and help facilitate a natural healing response. The cells may respond by a variety of mechanisms, which promote tissue survival, graft retention, and/or differentiation of progenitor cells into the appropriate cell type.
Then, during the face lift, the regenerative cells tissue embedded in fat is then gently placed with a blunt cannula in layers of facial tissues like the SMAS, under the muscles, etc…. Once the fat is placed, symmetry is checked and then the skin is redraped and approximated, the excess skin excised and then anchored in a vertical direction and closed in layers. The key is to place this regenerative tissue in a precise location in order to enhance the volume of the face in areas previously volume deprived.
After the cell-enhanced face lift, the patient exhibits a dramatic improvement not only in the underlying soft tissue contouring of the face but the skin itself. The growth factors contained in these cells induce the skin and the other tissues to produce more cells of their own by basically initiating a signal to the local stem cells as well as the transplanted adult stem cells to restore them self and multiply.
Others techniques of stem cell face lift inject the cells directly in the face,( without surgery) but in Dr. Calabria’s opinion is not as effective in voluminizing the face that the cell-enhanced ( stem cell) face lift and it does not address the laxity of the skin.
Also the cells have not been isolated with the celution device which Dr. Calabria thinks is essential to the final result.
The regenerative cells, by secreting growth hormone and other factors, are also beneficial to create a more youthful look, diminishing the aging process. The procedure restores the youthful contour and shape of the face as well as skin tightness and evens out color irregularities caused by aging and sun damage.
The cell-enhanced (stem cell) face lift is the new frontier of face lifting and Dr. Calabria is definitely writing a new chapter in facial rejuvenation.
The Celution device is not available in the US yet but has been approved for clinical use in Europe and it is available in Dr. Calabria’s Milan and Rome locations and he will bring the technology to the U.S. as soon as next year.
Find more information on Dr Calabria’s website www.drcalabria.com