AGE-RELATED MACULAR DEGENERATION (AMD)
What is AMD?
Age-related macular degeneration (AMD) is a disease that affects the macula, the part of the eye that allows a person to see fine detail. AMD gradually destroys the sharp, central vision, which is needed for seeing objects clearly, and for common daily tasks such as reading and driving.
AMD causes no pain and, in some cases, advances so slowly that people notice little change in their vision. In others, the disease progresses faster and may lead to a rapid loss of vision in both eyes. AMD is a leading cause of vision loss in the western world for individuals over the age of 60, and is thought to affect over three million people in the UK alone. AMD occurs in two forms: wet and dry.
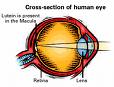
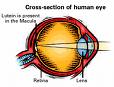
Where is the macula?
The macula is located in the centre of the retina – the light-sensitive tissue at the back of the eye. The retina instantly converts light into electrical impulses, known as nerve signals, and sends them on to the brain for image interpretation.
What is dry AMD?
Dry AMD occurs when the light-sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye. As dry AMD gets worse, a person may see a blurred spot in the centre of his or her vision. Over time, central vision is gradually lost in the affected eye.
The most common symptom of dry AMD is slightly blurred vision. A person may have difficulty recognising faces and may need more light for reading and other tasks. Dry AMD generally affects both eyes, but vision can be lost in one eye while the other eye seems unaffected. One of the most common early signs of dry AMD is drusen in the eye, possibly combined with pigment abnormalities.
What is drusen?
Drusen are yellow deposits under the retina often found in people over age 60, and in isolation do not normally cause vision loss. In fact, scientists are unclear about the connection between drusen and AMD, but have found that an increase in the size or number of drusen raises a person’s risk of developing either advanced dry AMD or wet AMD.
An eye care professional can detect drusen during a comprehensive dilated eye exam.
What is wet AMD?
Wet AMD is another advanced stage of AMD and is generally preceded by early or intermediate dry AMD. Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These new blood vessels tend to be very fragile and often leak blood and fluid. The blood and fluid raise the macula from its normal place at the back of the eye, and damage to the macula occurs rapidly.
With wet AMD, loss of central vision can occur quickly.
What are the stages of AMD?
AMD has three stages, all of which may occur in one or both eyes:
1. Early AMD – people with early AMD have either several small, or a few medium-sized drusen. At this stage, there are no other symptoms and no vision loss.
2. Intermediate AMD – people with intermediate AMD have either many medium-sized or one or more large drusen. Some people see a blurred spot in the centre of their vision. More light may be needed for reading and other tasks.
3. Advanced AMD – in addition to drusen, people with advanced dry AMD or advanced wet AMD have a breakdown of light-sensitive cells and supporting tissue in the central retinal area. This breakdown can cause a blurred spot in the centre of the vision. Over time, the blurred spot may get bigger and darker, taking more of the central vision. Individuals may have difficulty reading or recognising faces until they are very close.
If a person has vision loss from dry AMD in one eye only, he or she may not notice any changes in overall vision. With the other eye seeing clearly, the individual can still drive, read and see fine details, and may notice changes in vision only if AMD affects both eyes.
Which is more common – the dry form or the wet form?
The dry form is much more common, although scientists are still not sure what causes it. More than 85 per cent of all people with intermediate and advanced AMD combined have the dry form.
However, if only advanced AMD is considered, about two-thirds of patients have the wet form. Because almost all vision loss comes from advanced AMD, the wet form leads to significantly more vision loss than the dry form.
Can the dry form turn into the wet form?
Yes. All people who have the wet form of AMD had the dry form first. Dry AMD can advance and cause vision loss without turning into the wet form of the disease. The dry form also can suddenly turn into the wet form, even during early stage AMD. There is no way to tell if or when dry will turn into wet AMD.
The dry form has early and intermediate stages. Does the wet form have similar stages?
No. The wet form is considered advanced AMD.
Can advanced AMD be either the dry form or the wet form?
Yes. Both the wet form and the advanced dry form are considered advanced AMD, and vision loss can occur with either form, although in most cases, only advanced AMD can cause vision loss. People who have advanced AMD in one eye are at especially high risk of developing advanced AMD in the other eye.
Causes and Risk Factors
Who is at risk of developing AMD?
The greatest risk factor is age. Although AMD may occur during middle age, studies show that people over age 60 are clearly at greater risk than other age groups. For instance, a large study found that middle-aged people have about a two per cent risk of developing AMD, but this risk increased to nearly 30 per cent in those over age 75.
Other risk factors include:
Smoking – smokers have an increased risk of developing AMD
Family History – individuals with immediate family members who have AMD are at a higher risk of developing the disease
Obesity – research studies suggest a link between obesity and the progression of early and intermediate stage AMD to advanced AMD
Poor nutrition lacking in lutein /zeaxanthin rich diet (nutrients found in green leafy vegetables such as curly kale and egg yolk)
Race – Caucasians seem to be more likely to lose vision from AMD than those with darker skin
Gender – women appear to be at greater risk than men
Can a person’s lifestyle make a difference?
A person’s lifestyle can play a role in reducing the risk of developing AMD. So it’s important to remember to:
Eat a healthy diet that’s high in fruit, fish and vegetables, specifically green leafy vegetables
Avoid smoking
Maintain a normal blood pressure
Maintain a healthy weight and exercise regularly
Symptoms and Detection
What are the symptoms of AMD?
Dry AMD: The most common early sign for dry AMD is blurred vision. As fewer cells in the macula are able to function, people will see details such as faces or words in a book less clearly.
Often this blurred vision disappears in brighter light. If the loss of these light-sensing cells becomes great, people may see a small but growing blind spot in the middle of their field of vision.
Wet AMD: The classic early symptom for wet AMD is that straight lines appear crooked. This results when fluid from the leaking blood vessels gathers and lifts the macula, distorting vision. A small blind spot may also appear in wet AMD, resulting in loss of one’s central vision.
Neither dry nor wet AMD cause pain.
How is AMD detected?
An eye care professional may suspect AMD if the person is over age 60 and has had recent changes in central vision. AMD is detected during a comprehensive eye exam that includes a visual acuity test, dilated eye exam, and tonometry (a measurement of intraocular pressure).
An eye care professional also may perform other tests to learn more about the structure and health of the eye. For example during an eye exam, the patient may be asked to look at an Amsler grid a grid of straight lines with a black dot in the centre. The patient will be asked to cover one eye and stare at the black dot. While staring at the dot, they may notice that the straight lines in the pattern appear wavy, and that some of the lines are missing. These may be signs of AMD.
If an eye care professional believes the patient needs treatment for wet AMD, he or she will suggest a fluorescein and/or indocyanin green angiogram to identify any leaking blood vessels and recommend treatment.
What does AMD mean for the patient?
For many, AMD is a shock which can be compounded by lack of information, empathy and support available. Patients are frequently told that little can be done to treat the condition, leaving them feeling both angry and depressed.
People with AMD are more likely to become depressed than the general population, and depression can increase the difficulty of adjusting to the disease (Quality of life in age-related macular degeneration Royal Holloway University of London, 2006). Indeed, a US cross-sectional study of 151 patients living with AMD reported that the rate of depressive disorder was twice that generally found among elderly people living in the community.
Those living with AMD may lose their independence, requiring help with personal and household tasks and other aspects of daily life. Shopping, cooking and general mobility are also more difficult for people with AMD than those of a similar age with no visual impairment. An additional prospective study of AMD patients with recent (within six weeks) loss of vision to their second eye found that of the 51 participants, 33% met the criteria for clinical depression (a higher rate than 16% found in the wider community), of whom only one was receiving treatment for depression, suggesting low levels of pre-existing depression (Source: Rovner, Casten and Tasman Effect of depression on vision function in age-related macular degeneration (Journals of Ophthalmology, 2002).
Other health problems associated with age such as arthritis and osteoporosis serve to impair quality of life still further.
Visual hallucinations, known as Charles Bonnet Syndrome, and common in those with visual impairments, can also occur with AMD. While benign and frequently short-lived, research suggests that few are warned that AMD can cause hallucinations and may not report them, featuring dementia. Such unnecessary worry may further damage quality of life.
Rehabilitation, including the provision of low vision aids and training in their use, has been proven to benefit those with AMD, improving visual function and assisting quality of life. Psycho-social interventions, such as peer support groups, also help sufferers adjust to the disease.
Treatment
How is wet AMD treated?
Wet AMD can be treated with laser surgery, photodynamic therapy, and injections into the eye. None of these treatments are a cure for wet AMD, and the disease and loss of vision may progress despite treatment.
1. Laser surgery – this procedure, which is performed in a doctor’s office or eye clinic, uses a laser to destroy the fragile, leaky blood vessels. A high-energy beam of light is aimed directly onto the new blood vessels and destroys them, preventing further loss of vision.
However, laser treatment may also destroy some surrounding healthy tissue and some vision. Only a small percentage of people with wet AMD can be treated with laser surgery. It is more effective if the leaky blood vessels have developed away from the fovea, the central part of the macula.
The risk of new blood vessels developing after laser treatment is high. Repeated treatments may be necessary, and in some cases, vision loss may progress despite repeated treatments.
2. Photodynamic therapy – a drug called verteporfin is injected into the arm. It travels through the body, including the new blood vessels in the eye, and tends to “stick” to the surface of the new vessels.
Next, a light which activates the drug is beamed into the eye for around 90 seconds, which destroys the new blood vessels and leads to a slower rate of vision decline. Unlike laser surgery, this drug does not destroy surrounding healthy tissue. Because the drug is activated by light, the patient must avoid exposing skin or eyes to direct sunlight or bright indoor light for five days after treatment.
Photodynamic therapy slows the rate of vision loss, but does not stop it or restore vision in eyes already damaged by advanced AMD. Treatment results often are temporary and a person may need to be treated again. Photodynamic therapy is relatively painless, takes about 20 minutes and is normally performed in a dedicated hospital clinic.
3. Injections – wet AMD can now be treated with new drugs that are injected into the eye (anti-VEGF or anti-angiogenic therapy). Abnormally high levels of a specific growth factor occur in eyes with wet AMD and promote the growth of abnormal new blood vessels. This drug treatment blocks the effects of the growth factor.
A person will need multiple injections that may be given as often as every month. The eye is numbed before each injection, and the patient may need to remain in hospital for a period of time after each session for monitoring. This drug treatment can help slow down vision loss from AMD and in some cases improve sight.
How is dry AMD treated?
Once dry AMD reaches the advanced stage, no form of treatment can prevent vision loss. However, intake of certain antioxidant vitamins and zinc can delay and possibly prevent intermediate AMD from progressing to the advanced stage, in which vision loss occurs.
The US National Eye Institute’s Age-Related Eye Disease Study (AREDS) found that taking Bausch & Lomb’s PreserVision, a high-potency nutritional supplement containing antioxidants and zinc, significantly reduces the risk of advanced AMD and its associated vision loss. Slowing AMD’s progression from the intermediate stage to the advanced stage will save the vision of many people.
Age-Related Eye Disease Study (AREDS)
What is the dosage of the AREDS formulation?
The specific quantities of antioxidants and zinc used by the AREDS researchers were 500 milligrams of vitamin C; 400 International Units of vitamin E; 15 milligrams of beta-carotene (often labelled as equivalent to 25,000 International Units of vitamin A); 80 milligrams of zinc as zinc oxide; and two milligrams of copper as cupric oxide. Copper was added to the AREDS formulation containing zinc to prevent copper deficiency anaemia, a condition associated with high levels of zinc intake.
Bausch & Lomb’s PreserVision Original formulation, which was proven safe and effective by the AREDS study, is available in soft gel and tablet forms. The new PreserVision Lutein soft gels replace beta-carotene with lutein and are suitable for smokers.
Who should take the AREDS formulation?
People who are at high risk for developing advanced AMD should consider taking the formulation in consultations with their health care provider or personal physician. A person is at high risk of developing advanced AMD if he or she has either:
1. Intermediate AMD in one or both eyes.
-OR-
2. Advanced AMD (dry or wet) in one eye, but not the other.
The AREDS formulation is not a cure for AMD, nor will it restore vision already lost from the disease. However, it may delay the onset of advanced AMD. It may also help people who are at high risk of developing advanced AMD keep their vision.
Can diet alone provide the same high levels of antioxidants and zinc as the AREDS formulation?
No. High levels of vitamins and minerals are difficult to achieve from diet alone. However, previous studies have suggested that people who have diets rich in fruit, fish and vegetables, specifically, green leafy vegetables, have a lower risk of developing AMD.
Can a daily multi-vitamin alone provide the same high levels of antioxidants and zinc as the AREDS formulation?
No. The formulation’s levels of antioxidants and zinc are considerably higher than the amounts in any daily multi-vitamin. If a person is already taking daily multi-vitamins and his or her doctor suggests taking the high-dose AREDS formulation, it is recommended that the individual review all vitamin supplements with his or her doctor prior to taking the AREDS formulation.
Because multi-vitamins contain many important vitamins not found in the AREDS formulation, a person may wish to take a multi-vitamin along with the AREDS formulation. For example, people with osteoporosis need to be particularly concerned about taking vitamin D, which is not in the AREDS formulation.
How can a person take care of his or her vision once diagnosed with AMD?
If a person has dry AMD, he or she should have a comprehensive dilated eye exam at least once a year. An eye care professional can monitor his or her condition and check for other eye diseases. Also, if a person has intermediate AMD in one or both eyes, or advanced AMD in one eye only, the doctor may suggest that the individual take the AREDS formulation containing the high levels of antioxidants and zinc.
Because dry AMD can turn into wet AMD at any time, a person should obtain an Amsler grid from their eye care professional. It is recommended that the individual use the grid every day to evaluate his or her vision for signs of wet AMD. This quick test works best for people who still have good central vision. If a person detects any changes in the appearance of this grid or in his or her everyday vision while reading the newspaper or watching television, he or she needs a comprehensive dilated eye exam.
If a person has wet AMD, a doctor would normally advise immediate treatment. After laser surgery or photodynamic therapy or anti-VEGF anti-angiogenic therapy, a person will need frequent eye exams to detect any recurrence of leaking blood vessels.
Studies show that people who smoke have a greater risk of recurrence than those who don’t. In addition, a person should check his or her vision daily at home using the Amsler grid and will need to schedule an eye exam immediately if any changes are detected.
What can a person do if he or she has already lost some vision from AMD?
If a person has lost some sight from AMD, he or she should not be afraid to use his or her eyes for reading, watching TV, and other routine activities. Normal eye use will not cause further vision damage. These individuals should also ask their eye care professional about low-vision services and devices that may help make the most of their remaining vision.
Many community organisations and agencies offer information about low-vision counselling, training, and other special services for people with visual impairments. Macular Disease Society is of particular value to many existing AMD sufferers. The Royal National Institute of the Blind (RNIB) also provides support and services for those experiencing vision difficulties and loss.
Current Research
What AMD research is currently being conducted?
Research is conducted globally to help provide better ways to detect, treat, and prevent vision loss through AMD. Currently, scientists are:
Studying the possibility of transplanting healthy cells into a diseased retina – a London-based project to cure AMD has recently been launched, following £4 million donation from an anonymous American donor. This will involve a study where patients will be treated for dry AMD with injections of Retinal Pigment Epithelium (RPE) into the eye. The RPE itself has been developed under laboratory conditions from embryonic stem cells. The study is likely to take at least five years to complete, and will be undertaken by Moorfields Eye Hospital in conjunction with the Institute of Ophthalmology at University College London and the University of Sheffield
Evaluating families with a history of AMD to understand genetic and hereditary factors that may cause the disease
Looking at certain anti-inflammatory treatments for the wet form of AMD
AREDS II further examining the role of vitamins, lutein, omega-3 fatty acids and zinc