The risk of blood clots caused by hormone replacement is lower in women who use natural bioidentical substitutes, reveals new research.
 In an article published in the medical journal, JAMA Internal Medicine, researchers investigated 384 postmenopausal women taking part in the Heart and Vascular Health Study, a study of cardiovascular events involving subjects between the ages of 30 to 79 years.
In an article published in the medical journal, JAMA Internal Medicine, researchers investigated 384 postmenopausal women taking part in the Heart and Vascular Health Study, a study of cardiovascular events involving subjects between the ages of 30 to 79 years.
The patients had used oral “conjugated equine estrogens” (CEE’s) or estradiol from 2003 to 2009. Sixty-eight women who had experienced venous thrombosis (deep vein thrombosis or pulmonary embolism), 67 women who had undergone a heart attack and 48 subjects who had an ischemic stroke were matched for age and other factors with 201 control subjects. lower risk of venous blood clots in association with the use of orally administered bioequivalent estradiol in comparison with CEEs, marketed under the name of Premarin®for the treatment of menopausal symptoms.
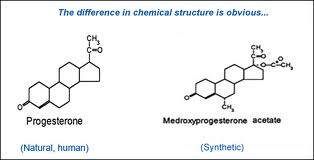
“Pharmaceutical estrogens are molecularly distinct,” write authors Nicholas L. Smith, PhD and his colleagues. “Conjugated equine estrogens are manufactured from the urine of pregnant mares and contain 10 known biologically active estrogen compounds, as well as others that have yet to be described. The primary compounds are estrone and equilin sulfate. Estradiol is a ‘natural’ or ‘bioequivalent’ estrogen.”
Among women who used CEEs, the risk of experiencing venous thrombosis (blood clots) was more than double that of subjects who used estradiol. Conjugated equine estrogen users also experienced a greater risk of heart attack which did not reach statistical significance. Analysis of plasma samples from 140 control subjects also indicated stronger propensity for blood clotting among those who used CEEs.
“Although oral estrogens are effective for managing menopause symptoms, not enough is known about the cardiovascular safety of different oral hormone therapy products relative to each other,” noted Dr Smith, who is a professor of epidemiology at the University of Washington School of Public Health in Seattle. “If our results are confirmed, women seeking menopausal treatment and their providers would find this information helpful when selecting a drug.”
